Everything you need to know about pancreatitis
Pancreatitis is a serious condition that affects many individuals worldwide. Understanding this ailment, its symptoms, causes, and treatment is crucial for those at risk.
This article aims to provide everything you need to know about pancreatitis, ensuring that readers are informed and prepared to seek help when necessary.
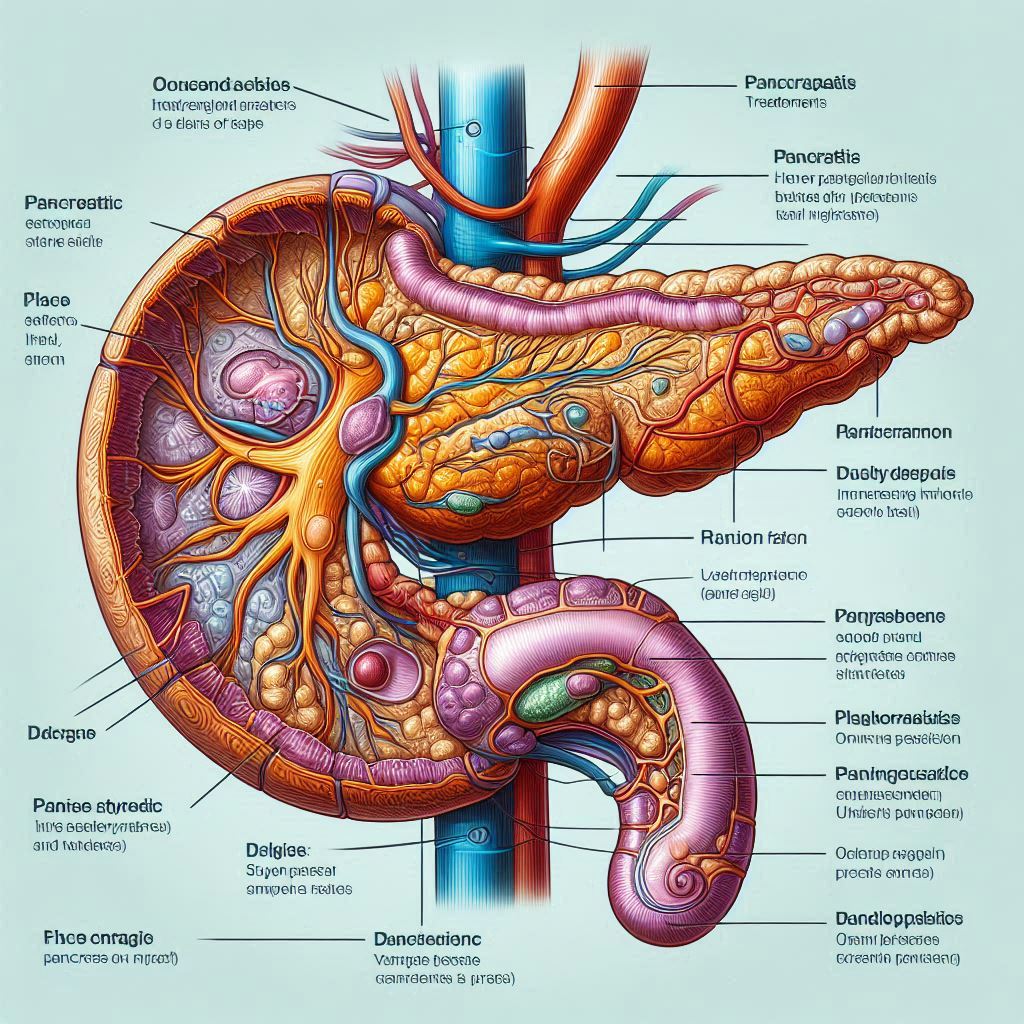
What is pancreatitis?
Pancreatitis is defined as the inflammation of the pancreas, an essential organ that plays a vital role in digestion and blood sugar regulation. This condition can be categorized into two main types: acute and chronic.
Acute pancreatitis is characterized by sudden inflammation that can lead to severe abdominal pain, nausea, and vomiting. Often requiring hospitalization, this type of pancreatitis can improve quickly with appropriate medical care.
Chronic pancreatitis, on the other hand, is a long-term condition that develops gradually and can result in permanent damage to the pancreas. In many cases, it is associated with other health issues, such as diabetes.
What are the symptoms of pancreatitis?
Symptoms of pancreatitis can vary depending on whether it is acute or chronic. For acute pancreatitis, common symptoms include:
- Severe abdominal pain that may radiate to the back
- Nausea and vomiting
- Fever
- Rapid pulse
Chronic pancreatitis symptoms may differ somewhat, often including:
- Persistent abdominal pain
- Diarrhea or oily stools
- Weight loss despite normal eating
- Signs of diabetes
Recognizing these symptoms early can be crucial for effective treatment and management of the condition.
What causes pancreatitis?
The causes of pancreatitis can be multifaceted. The most common triggers include:
- Gallstones: These small stones can block the pancreatic duct, leading to inflammation.
- Alcohol consumption: Excessive drinking is a significant risk factor for developing both acute and chronic pancreatitis.
- Medications and certain medical conditions, such as cystic fibrosis, can also contribute to the development of pancreatitis.
Understanding these causes is vital for prevention and for managing risk factors associated with pancreatitis.
When should I see my doctor about pancreatitis?
If you experience symptoms such as severe abdominal pain, persistent nausea, or vomiting, it is essential to seek medical attention. These could be signs of acute pancreatitis, which may require immediate treatment.
Furthermore, if you have a history of pancreatitis and begin to notice a change in your symptoms, such as increased pain or digestive issues, consult your doctor promptly.
Early intervention can be crucial in preventing complications associated with pancreatitis, such as necrotizing pancreatitis or the formation of pseudocysts.
How is pancreatitis diagnosed?
Diagnosis of pancreatitis typically involves a combination of tests and evaluations. Initially, a healthcare provider will conduct a thorough medical history and physical examination.
Blood tests are essential in diagnosing pancreatitis, as they can reveal elevated levels of pancreatic enzymes, indicating inflammation. Additionally, imaging tests like CT scans or ultrasounds may be performed to assess the severity of the condition.
These diagnostic methods are crucial in determining the appropriate treatment plan for those affected by pancreatitis.
How is pancreatitis treated?
Treatment options for pancreatitis largely depend on its severity and underlying causes. For acute pancreatitis, hospitalization may be necessary. Treatment often includes:
- Intravenous (IV) fluids to prevent dehydration
- Pain management with medications
- Dietary changes, often starting with a clear liquid diet
Chronic pancreatitis management may involve long-term dietary adjustments, enzyme replacement therapy, and regular monitoring for complications. In some cases, surgery may be required to address complications from chronic pancreatitis.
Can pancreatitis be prevented?
The prevention of pancreatitis largely hinges on lifestyle choices. Some effective strategies include:
- Avoiding excessive alcohol consumption
- Maintaining a healthy weight
- Eating a balanced diet low in fat
By managing these risk factors, individuals can significantly reduce their likelihood of developing pancreatitis in the future.
What not to do when you have pancreatitis?
When dealing with pancreatitis, it is crucial to avoid certain actions that can exacerbate the condition. First and foremost, you should refrain from consuming alcohol, as it can lead to further inflammation of the pancreas.
Additionally, it is advisable to avoid high-fat foods, as they can worsen digestive issues and increase abdominal pain. Ignoring symptoms and delaying medical attention can also have serious consequences, so it is essential to seek help if symptoms worsen.
What is the red flag for pancreatitis?
A significant red flag for pancreatitis is the experience of severe abdominal pain that persists or worsens over time. This pain often has a sudden onset and can be accompanied by symptoms such as nausea and vomiting.
Other concerning signs include fever and rapid heartbeat, which may indicate complications. If you notice these symptoms, it is vital to seek immediate medical assistance to prevent more severe health issues.
Is pancreatitis very serious?
Yes, pancreatitis can be a very serious condition. Acute pancreatitis can lead to life-threatening complications, such as organ failure or infection. Chronic pancreatitis can result in long-term damage and can significantly impact quality of life.
Furthermore, complications from pancreatitis can include diabetes, malnutrition, and pancreatitis-related cancer. This highlights the importance of early diagnosis and treatment to mitigate risks.
What helps pancreatitis go away?
For acute pancreatitis, treatment typically focuses on managing pain and allowing the pancreas to heal. This may include hospitalization, IV fluids, and a temporary halt to eating to minimize stress on the pancreas.
Chronic pancreatitis management often requires ongoing care, including dietary changes, enzyme supplements, and pain management strategies. Adhering to a healthy lifestyle is essential in helping the pancreas recover and function optimally.
Recognizing and managing the symptoms effectively, along with regular medical check-ups, can significantly improve outcomes for those experiencing pancreatitis.

Leave a Reply